Comparison of Photochemical Tissue Binding using Rose Bengal Dye and Skin Sutures for Closure of Incisional Cutaneous Wound in a Rabbit Model
Ambrina Tariq1
Arsalan Khan2*
Ghulam Jelani3
1,2Livestock & Dairy Development (Department), Khyber Pakhtunkhwa, Peshawar-25000-Pakistan |
AbstractWound healing is a complicated series of inter-related events which are mediated in their diverse phases in a broad range of cellular processes coordinated chemically as well as hormonally. It is typified by sequence of self-determining and overlapping events. Traditional wound closure methods, such as staples and sutures, have numerous drawbacks, including the possible occurrence of inflammation, irritation, infection, wound gapes, and leakage. The present study was therefore designed to evaluate the efficacy and potential of photochemical tissue bonding in the wound healing. For this purpose, 20 adult healthy, rabbits of either sex were selected. A full thickness incised wound on ventral midline was created on each rabbit. In animals of group A, incised wounds were exposed to monochromatic green light (532 nm) after application of dye (Rose Bengal) on the wound surface for 200 seconds whereas in group B the closure of the wounds were carried out using 2/0 silk suture material by interrupted horizontal mattress pattern. Healing was checked on daily basis through observation and measurements. There was a significant difference in swelled areas of wounds sutured by silk and healed with PTB. When horizontal mattress pattern was used, swelling of sutured area was significantly more prominent with silk .Among two wound closing techniques, more swelled area was observed in wounds sutured with horizontal mattress than the wounds closed with PTB. The healing time of photochemical tissue bonding treated wounds were 3 to 4 days while the healing time in sutures was 7 days. According to the histopathological evaluation of the collagen fibers photochemical tissue bonding resulted in a significantly dense collagen fiber as compared to the conventional suturing for closure of skin wounds in rabbits. Photochemical tissue bonding resulted in a collagen contents of 82.17±1.8 whereas in conventional suturing 78.50±1.5 collagen contents were observed. Photochemical tissue bonding resulted in epidermis thickness 125.1 ± 6.5 whereas in conventional suturing the epidermis thickness was 116.2 ± 3.1. Photochemical tissue bonding resulted in a dermis thickness of 120.9 ±7.7 whereas the thickness of dermis in conventional suturing was 113.7 ± 5.6.``` |
Licensed: |
|
Keywords: |
|
| (* Corresponding Author) |
Funding: This study received no specific financial support. |
Competing Interests:The authors declare that they have no competing interests. |
1. Introduction
Open wounds are generally physical, chemical or thermal injuries which results in breakage in the continuity of soft tissues. Therefore, the skin continuity should be restored. For this purpose, proper methods used for wound healing are necessary for re-establishment of skin. The normal histological and anatomical functions which have lost due to the breakage of the direct connection of the tissues of the skin then come towards its normal functions after healing [1].
In animals and men, cutaneous wounds are most commonly encountered throughout the world. In response to the wound, the body restores a process of healing which encloses various complex physiological phases of hemostasis, inflammation and proliferation as development of granulation and remodeling of tissues. All the events of healings occur at an optimum rate among the normal healthy individuals [2]. After a few hours of injury, granulation tissues are formed at the site of injury and also re-epithelization starts which subsequently covers the site of injury [3].
Wound healing process is very important for the closure of wound. Immediately after the damage the hemostasis phase of the healing initiates in which the development of fibrin and degranulation of platelets occur. Then after injury, inflammation stage commences. In this stage, removal of the injured tissues and bacteria from the wound is carried out by the recruitment of the constituent of the immune system. After that, tissue formation stage or the proliferative stage begins in which re-epithelization of injured tissues, proliferation of the fibroblast and endothelial cells occurs. In last remodeling stage, final growth of mature collagen type I occurs and this stage may take as long as 6-12 months after injury. In the duration of wound healing process, the wound strength progressively increases [4].
Various types of suture materials and suturing techniques are used in surgery and wound closure like sutures, clips, staples, skin closure bands, or topical pastes. Suture materials and pattern to be applied depends on wound type, location, skin and tissue thickness and degree of tension which can also affect the healing process [5]. Likewise, patterns for suturing are categorized according to their way of appointment as continuous or interrupted, while on the basis of the effects on the periphery of wound, the pattern may be inverting, everting or appositional [3].
Wound closure methods as traditional, staples and sutures. These have numerous drawbacks which includes possible occurrence of inflammation, irritation, infection, wound gapes, and leakage. In corneal applications, due to uneven suture tension sutures often produce astigmatism. Undesirable results are produced in the cosmetic use of staples and sutures [6].
Others possible alternatives to sutures and staples includes hemostatic adhesives such as fibrin sealants [7] cyanoacrylate adhesives and photodynamic tissue glue, which is composed of a mixture of riboflavin-5-phosphate and fibrinogen, which has been reported to close cataract incisions and attach donor cornea in corneal transplantation [8].
In addition to these methods of tissue binding, temperature-controlled tissue binding has also been reported in cornea of bovine and intestine of rat. Photochemical tissue binding of dura mater has also been an emerging technique which has been reported, using 1, 8 naphthalimides irradiated with visible light [7].
One of wound healing techniques is photochemical tissue bonding (PTB) technique in which photosensitizing dye is activated by the light energy and produces the chemical reactions which result in tissue repair and chemical bonding subsequently. Photochemical tissue bonding technique has intrinsic advantages over the thermal mechanisms because PTB does not need tight control of dosimetry because a specified temperature is not required and by evading elevated temperatures entailed in thermal welding, denaturation can also be avoided and the structural association of the tissues can be retained [9].
Photochemical tissue binding methods includes the application of a photosensitizer to a tissue, e.g., cornea as followed by irradiation with electromagnetic energy to produce a tissue seal. These methods are most useful in wound repairing [6].
2 Materials and Methods
2.1. Experimental Animals
A total of 20 adult healthy rabbits of both sex were procured from the local market. They were selected for the comparative effects of sutures and photochemical tissue bonding (PTB) on incised skin wound healing in rabbit model. All animals were managed indoor uniformly during the research period. Each animal was considered as a single experimental model. Uniform feeding and proper management conditions were provided to each animal during the study period. For identification purpose, the experimental animals were marked with the black permanent marker on the inside of the ear.
2.2. Infliction of Wound on Ventral Midline
The rabbits were anesthetized, surgical area where the incision was made was disinfected, hairs were clipped, after this the clean surgical blade was placed in the scalpel and the wound was produced on mid ventral line.
2.3.Treatment Procedure
The rabbits were divided into two groups; viz Group A with 10 rabbits, in which the wound was treated using PTB (application of RB dye + exposure of 532nm monochromatic green light) after application of dye (RB) on the wound surface for 200 seconds and Group B with 10 rabbits, in which the wound was treated using 2/0 silk suture material and interrupted horizontal mattress suture pattern.
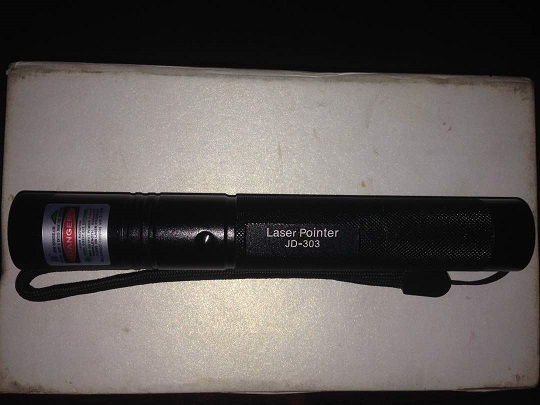
Plate-1. Monochromatic green light (532 nm wavelength) used to induce PTB.
2.4. Evaluation Parameters
To evaluate wound healing efficacy of PTB as compared to sutures following parameters were recorded.
- Healing score
- Healing time
- Tensile strength
- Histopathological evaluation
3. Results
In surgery, different types of suturing techniques like clips, staples, skin closure bands and topical pastes and different suture materials including absorbable and non-absorbable suture threads were used. Literature depicts a lot of studies on suture materials and techniques but less information is available regarding effects of photochemical tissue bonding PTB and conventional suturing techniques on cutaneous wound healing in veterinary practice. Therefore, the current study has been designed to compare the morphological characteristics and outcome of incised skin wounds closed with photochemical tissue bonding PTB using Rose Bengal Dye (RB) and a monochromatic green light with a wavelength of 532 nm and skin sutures with silk by interrupted horizontal mattress pattern. A total of 20 rabbits were randomly divided into 2 equal groups. Incised skin wounds were created on ventral midline. In animals of group A, the wounds were closed with PTB by staining the wound with RB dye and exposed it to monochromatic green light 532 nm for 200 seconds. In the rabbits of group B, wounds were sutured with silk by using the interrupted horizontal mattress pattern. In clinical assessments, healing score were categorized as: excellent, good and fair. Healing time was noticed between the creations of wound till the scar was fallen off in both of the groups A and B. Tensile strength was checked to evaluate the degree of integrity and healing of PTB treated and sutured treated wounds. Histopathology was performed at day 3rd and 7th post-surgery by selecting the animals randomly from each group.
3.1. Healing Score
The healing score was categorized as excellent, good and fair. Regarding healing score photochemical tissue bonding (PTB) resulted in a significantly better healing score as compared to conventional suturing for wound closure in rabbits Figure 4.1. Photochemical tissue bonding resulted in a healing score of 2.8 ± 0.13 whereas the counterpart (suturing) produced a healing score of 1.8 ± 0.2 Table 1.
Table-1. Healing score (Mean ± SE) of two groups viz. Photochemical tissue bonding and conventional suturing in rabbits (n=20). Healing Score. |
| Treated Groups | Mean ± SE |
| Photochemical tissue bonding treated group | 2.8±0.13 |
| Sutured treated group | 1.8±0.20 |

Plate-2. Photograph showing outstanding healing score by PTB with no dehiscence and minimum inflammation. |

Plate-3. Cutaneous wound healing using simple interrupted suture pattern using Silk (2/0; Ethicon) suture material. |
3.2. Healing Time
Healing time (days) is the time elapse between the creation of the wound to the complete healing of the skin even when the scarring was occurred. It was estimated by sum of daily observations till scar is fallen off. Regarding healing time photochemical tissue bonding resulted a significantly faster healing time in days as compared to the conventional suturing for skin wound closure in rabbits Figure 4.2. Photochemical tissue bonding resulted in a healing time of 2.8 ± 0.74 days whereas the conventional suturing produced a healing time of 9.1 ± 1.91 days Table 2.
Table-2. Healing Time (Days; Mean ± SE) of two groups viz Photochemical Tissue Bonding (PTB) and conventional suturing in rabbit (n=20). |
| Treatment Groups | Healing Time ( Mean ± SE ) |
| PTB group | 2.8 ± 0.74 |
| Suturing group |
|
Source: Findings of this Research Trial |
3.3. Tensile Strength
Breaking strength/tensile strength of healed wound/tissue represents the degree of integrity and healing. Breaking strength was determined through tensometer. On complete healing of the tissue, tensile strength of regenerated tissue was measured by tensile testing machine (tensometer).The breaking strength measured between the photochemical tissue bonding and the conventional suturing was the 77.79±1.9 and 71.98±1 respectively Table 3 There was statistically significant difference between the breaking strength of photochemical tissue bonding and the conventional suturing.
Table-3. Breaking strength of two groups viz photochemical tissue bonding and conventional suturing in rabbits (n=20). |
| Treated groups | Breaking Strength (Mean ± SE) |
| PTB group | 77.79±1.9 |
| Suture group | 71.98±1 |
Source: Findings of this Research Trial. |
3.4. Histopathological Evaluation
According to the histopathological evaluation of the collagen fibers photochemical tissue bonding resulted in significantly dense collagen fibers as compared to the conventional suturing for closure of skin wounds in rabbits Figure 4.4. Photochemical tissue bonding resulted in a collagen contents of 82.17±1.8 whereas in conventional suturing 78.50±1.5 collagen contents were observed Table 4.
Table-4. Collagen fibers (Mean ± SE) of two groups viz of photochemical tissue bonding and suturing in rabbits (n=20). |
| Treated Groups | Collagen Content (Mean ± SE) |
| PTB group | 82.17±1.8 |
| Suture group | 78.50±1.5 |
Source: Findings of this Research Trial. |
3.5. Thickness of Epidermis
Regarding thickness of epidermis photochemical tissue bonding resulted in a significantly thickened epidermis as compared to the conventional suturing for skin wound closure in rabbit. Photochemical tissue bonding resulted in epidermis thickness 125.1 ± 6.5 whereas in conventional suturing the epidermis thickness was 116.2 ± 3.1 Table 5. The histopathological slide showed more leucocytic infiltration. Re-epithelization was more prominent and regular. Wounded portion was seen as normal. Prominent keratinization was found as compared to silk.
Table-5. Thickness of epidermis (Mean ± SE) of two groups viz photochemical tissue bonding and conventional suturing in rabbits (n=20). |
| Treated groups | Mean ± SE |
| PTB group | 125.1 ±6.5 |
| Suture group | 116.2± 3.1 |
Source: Findings of this Research Trial. |
3.6. Thickness of Dermis
Regarding dermis thickness photochemical tissue bonding resulted in a significantly thickened dermis as compared to the conventional suturing for wound closure in rabbits. Photochemical tissue bonding resulted in a dermis thickness of 120.9 ±7.7 whereas the thickness of dermis in conventional suturing was 113.7 ± 5.6 Table 6.
Table-6. Thickness of epidermis (Mean ± SE) of two groups viz photochemical tissue bonding and conventional suturing in rabbits (n=20). |
| Treated groups | Mean ± SE |
| PTB group | 120.9 ±7.7 |
| Suture group | 113.7 ± 5.6 |
Source: Findings of this Research Trial. |
4. Discussion
Wounds are generally the separating of the soft tissues in both the animals and the human. The healing of the wound is a complicated variety of co-related actions which are preceded in their diverse procedures in a broad variety of cellular processes interlinked chemically and hormonally. It is typified by a series of self-determining and clumping series [10].
One of wound healing techniques is photochemical tissue bonding (PTB) technique in which photosensitizing dye is activated by the light energy and produces the chemical reactions which result in tissue repair and chemical bonding subsequently. Photochemical tissue bonding technique has intrinsic advantages over the thermal mechanisms because PTB does not need tight control of dosimetry because a specified temperature is not required, and by evading elevated temperatures entailed in thermal welding, denaturation can also be avoided and the structural association of the tissues can be retained [9].Photochemical tissue binding methods include the application of a photosensitizer to a tissue, e.g., cornea, followed by irradiation with electromagnetic energy to produce a tissue seal. The methods are useful for wound repair, or other tissue repair [6].
The current study was designed to evaluate the efficacy and potential of photochemical tissue bonding in the wound healing. For this purpose, 20 adult healthy, rabbits of either sex were selected. A full thickness incised wound on ventral midline was created on each rabbit. In animals of group A, incised wounds were exposed to monochromatic green light (532 nm) after application of dye (Rose Bengal) on the wound surface for 200 seconds whereas in group B the closure of the wounds were carried out using 2/0 silk suture material by interrupted horizontal mattress pattern. Healing was checked on daily basis through observation and measurements. The evaluation criteria were based on clinical assessment score, healing time, tensile strength and histo-pathological evaluation. The data thus generated were analyzed by using appropriate statistical design.
Regarding healing score photochemical tissue bonding (PTB) resulted in a significantly better healing score as compared to conventional suturing for wound closure in rabbits. Photochemical tissue bonding resulted in a healing score of 2.8 ± 0.13 whereas the counterpart (suturing) produced a healing score of 1.8 ± 0.2.
Regarding healing time photochemical tissue bonding resulted a significantly faster healing time in days as compared to the conventional suturing for skin wound closure in rabbits. Photochemical tissue bonding resulted in a healing time of 2.8 ± 0.74 days whereas the conventional suturing produced a healing time of 9.1 ± 1.91 days. The findings of the study are in accordance with the findings reported by Capon, et al. [11] who have reported a four times faster healing time with laser as compared to conventional suturing. This may be attributed to less inflammatory process produced by the Laser treatment as compared to conventional suturing which are believed to be producing pronounced inflammatory reaction.
The breaking strength measured between the photochemical tissue bonding and the conventional suturing was the 77.79±1.9 and 71.98±1 respectively. There was statistically significant difference between the breaking strength of photochemical tissue bonding and the conventional suturing. The findings of the study are in accordance with the findings reported by Capon, et al. [11] and Poppas, et al. [12] who have reported a higher tensile strength with the laser than the conventional suturing. This may be attributed to denser collagen fibers and less space between the collagen fibers and increased thickness of dermis.
According to the histopathological evaluation of the collagen fibers photochemical tissue bonding resulted in significantly dense collagen fibers as compared to the conventional suturing for closure of skin wounds in rabbits. Photochemical tissue bonding resulted in a collagen contents of 82.17±1.8 whereas in conventional suturing 78.50±1.5 collagen contents were observed. The finding of the study are in accordance with the findings reported by Medrado, et al. [13] and Poppas, et al. [12] who have reported more collagen fibers deposition in the tissues healed by laser after 2,3,5 and 7 days as compared to conventional suturing. This may be due to proper leucocytic infiltration.
The Regarding thickness of epidermis photochemical tissue bonding resulted in a significantly thickened epidermis as compared to the conventional suturing for skin wound closure in rabbit. Photochemical tissue bonding resulted in epidermis thickness 125.1 ± 6.5 whereas in conventional suturing the epidermis thickness was 116.2 ± 3.1.Regarding dermis thickness photochemical tissues bonding resulted in a significantly thickened dermis as compared to the conventional suturing for wound closure in rabbits. Photochemical tissue bonding resulted in a dermis thickness of 120.9 ±7.7 whereas the thickness of dermis in conventional suturing was 113.7 ± 5.6.The finding of the study are in accordance with the findings reported by Simhon, et al. [14] who have reported more re-epitheization of tissues in laser treated healed wound as compared to conventional suturing. This may be due to re-colonization of the cells the cells are arranged in a close manner.
5. Conclusion
The findings of the study revealed that PTB had superior wound closure characteristics compared to conventional sutures as there was less inflammation, wound dehiscence and other post operative complications. PTB can be a potential alternative for wound closure than suturing as it requires less effort, less time and fewer resources, but a comprehensive experimental trial is required to evaluate its various merits along with demerits like tissue toxicity etc.
References
[1] R. S. Barreto, R. L. Albuquerque-Junior, A. A. Araujo, J. R. Almeida, M. R. Santos, A. S. Barreto, J. M. DeSantana, P. S. Siqueira, J. S. Quintans, and L. J. Quintans-Junior, "A systematic review of the wound-healing effects of monoterpenes and iridoid derivatives," Molecules, vol. 19, pp. 846-862, 2014.
[2] A. H. Kwon, Z. Qiu, and Y. Hirao, "Topical application of plasma fibronectin in full-thickness skin wound healing in rats," Experimental Biology and Medicine, vol. 232, pp. 935-941, 2007.
[3] J. Hochberg, K. M. Meyer, and M. D. Marion, "Suture choice and other methods of skin closure," Surgical Clinics, vol. 89, pp. 627-641, 2009.
[4] J. P. Rubin, J. P. Hunstad, A. Polynice, J. A. Gusenoff, T. Schoeller, R. Dunn, and J. E. Hansen, "A multicenter randomized controlled trial comparing absorbable barbed sutures versus conventional absorbable sutures for dermal closure in open surgical procedures," Aesthetic Surgery Journal, vol. 34, pp. 272-283, 2014.
[5] L. Mulroy, J. Kim, I. Wu, P. Scharper, S. A. Melki, D. T. Azar, and I. E. Kochevar, "Photochemical keratodesmos for repair of lamellar corneal incisions," Investigative Ophthalmology & Visual Science, vol. 41, pp. 3335-3340, 2000.
[6] I. E. Kochevar, C. R. Taylor, and J. Krutmann, Fundamentals of cutaneous photobiology and photoimmunology in Fitzpatrick’s dermatology in general medicine, Wolff K editor; Katz S, editor, 7th ed. New York, NY: McGraw-Hill, 2008.
[7] P. Henrick, S. Cowman, M. Winofrad, and M. Marion, "J Cataract Refract Surg," vol. 55, pp. 1-553, 1987.
[8] K. M. Goins, J. Khadem, and P. A. Majmudar, "Relative strength of photodynamic biologic tissue glue in penetrating keratoplasty in cadaver eyes," Journal of Cataract & Refractive Surgery, vol. 24, pp. 1566-1570, 1998.
[9] R. W. Redmond, C. Amann, B. P. Chan, W. A. Farinelli, R. R. Anderson, D. T. Azar, T. S. Johnson, J. Winograd, and M. A. Randolph, "Photochemical tissue bonding: Photons for healing," vol. 109, pp. 1-13, 2004.
[10] E. W. C. Chan, Y. Y. Lim, L. F. Wong, F. S. Lianto, S. K. Wong, K. K. Lim, and T. Y. Lim, "Antioxidant and tyrosinase inhibition properties of leaves and rhizomes of ginger species," Food Chemistry, vol. 109, pp. 477-483, 2008.
[11] A. Capon, E. Souil, B. Gauthier, C. Sumian, M. Bachelet, B. Buys, B. S. Polla, and S. Mordon, "Laser assisted skin closure (LASC) by using a 815-nm Diode-Laser system accelerates and improves wound healing," Lasers in Surgery and Medicine, vol. 28, pp. 168-175, 2001.
[12] D. P. Poppas, E. J. Wright, P. D. Guthrie, L. T. Shlahet, and A. B. Retik, "Human albumin solders for clinical application during laser tissue welding," Lasers in Surgery and Medicine: The Official Journal of the American Society for Laser Medicine and Surgery, vol. 19, pp. 2-8, 1996.
[13] A. R. Medrado, L. S. Pugliese, S. R. A. Reis, and Z. A. Andrade, "Influence of low level laser therapy on wound healing and its biological action upon myofibroblasts," Lasers in Surgery and Medicine, vol. 32, pp. 239-244, 2003.
[14] D. Simhon, T. Brosh, M. Halpern, A. Ravid, T. Vasilyev, N. Kariv, and Z. Nevo, "Closure of skin incisions in rabbits by laser soldering: I: Wound healing pattern," Lasers in Surgery and Medicine: The Official Journal of the American Society for Laser Medicine and Surgery, vol. 35, pp. 1-11, 2004.